Pathology Case of the Month - Eastern Massasauga Rattlesnake
Case History: An adult female eastern massasauga rattlesnake (Sistrurus catenatus) was found acting lethargic during species surveys in Wisconsin, U.S.A. and died the same day. Snake fungal disease (SFD) had previously been confirmed at this site, and another eastern massasauga found during the surveys exhibited skin lesions suggestive of SFD.
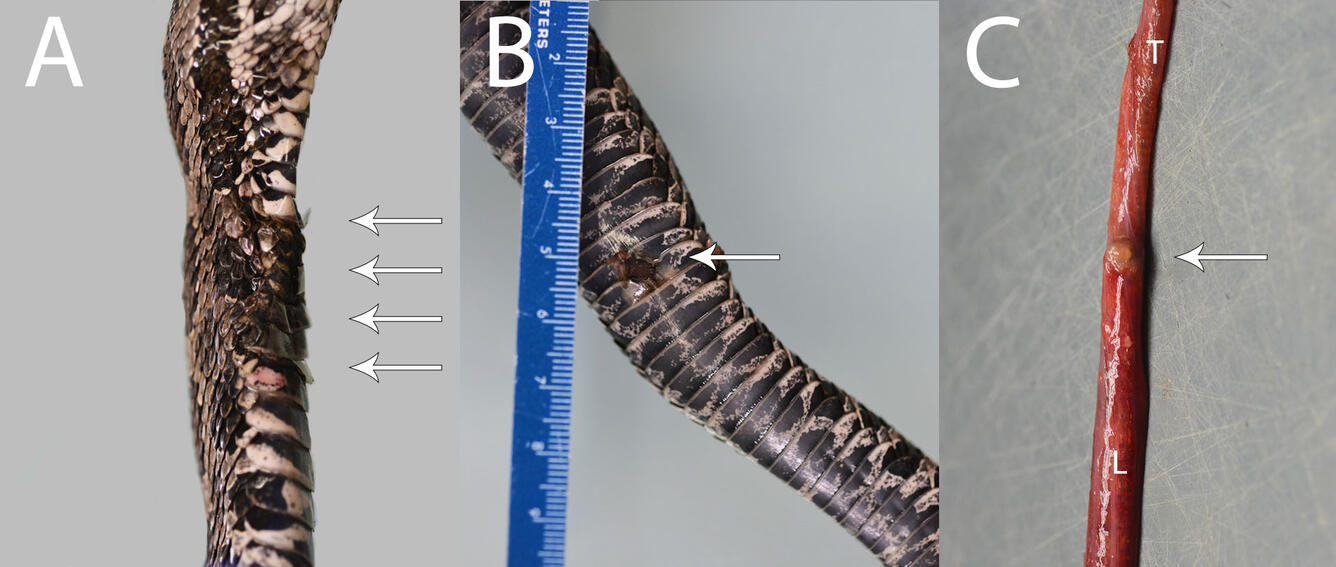
Gross Findings: The snake is in fair body condition with mild depletion of fat bodies. On the skin of the ventral and lateral neck and body are several areas of firm, tan-brown raised or depressed scales ranging from 4 x 6 mm to 15 x 12 mm (Figure 1A and B). The left lung is multifocally dark red. On the surface of the proximal lung is a 2 x 2 x 1 mm tan nodule (Figure 1C). Portions of lung sink in formalin.
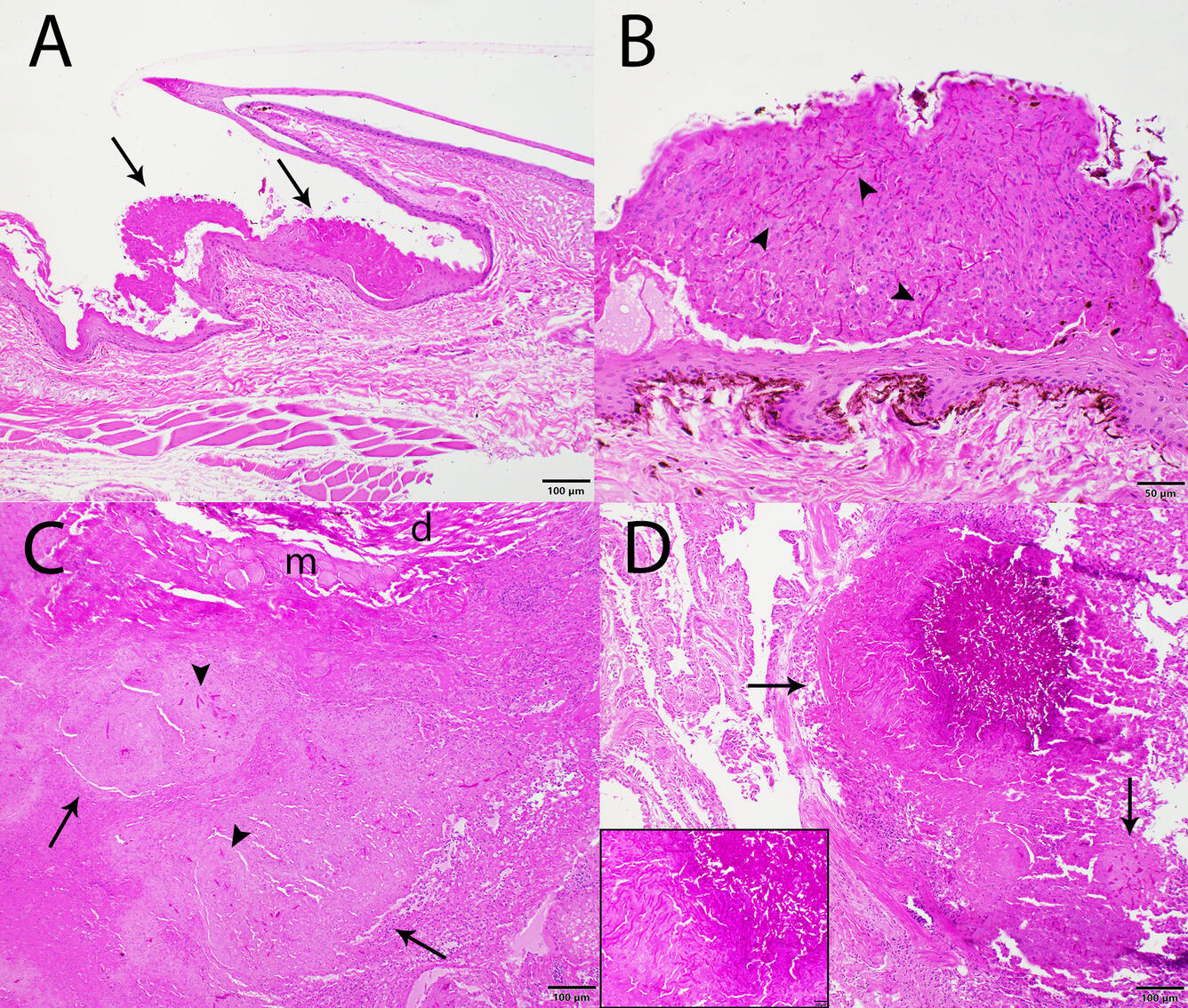
Histopathological Findings: On the head and ventral neck are mutifocal areas of superficial to mid-epidermal necrosis (Figure 2A and 2B). Necrotic areas contain variable numbers of ~5-µm diameter branching, septate, PAS-positive fungal hyphae (Figure 2B). The dermis contains multifocal accumulation of mononuclear cells. In few areas, fungal hyphae infiltrate the dermis and underlying skeletal muscle, with formation of multifocal granulomas containing fungal hyphae (Figure 2C). Within the lung is a focally extensive area with replacement of faveoli by similar fungal granulomas (Figure 2C).
Morphologic diagnoses:
- Skin: Epidermal necrosis, multifocal, moderate to marked, with intralesional fungal hyphae
- Skeletal muscle: Granulomas, multifocal, moderate to marked, with intralesional fungal hyphae
- Lung: Granulomas, focally extensive, moderate to marked, with intralesional fungal hyphae
Diagnostic test results:
Skin and lung, Ophidiomyces ophidiicola PCR: Detected
Skin, fungal culture: Ophidiomyces ophidiicola
Disease: Snake fungal disease (SFD)
Etiology: Ophidiomyces ophidiicola, a keratinophilic ascomycete fungus
Distribution: In free-ranging snakes, O. ophidiicola is primarily found in eastern United States, Canada and Europe, although it can occur in captive snakes worldwide. Ophidiomyces ophidiicola is suspected to have been introduced to the United States multiple times over the past few hundred years.
Seasonality: Infection can be seen at any time of year. In northern latitudes, it is more common in snakes that have recently emerged from hibernation, while in the deep south it is more common in winter.
Host range: Ophidiomyces ophidiicola has a broad host range and has been documeted in over 30 species of snakes. It has not been documented as infecting any non-snake species in the wild, although infection trials have demonstrated its ability to cause skin lesions in bearded dragons (Pogona vitticeps).
Transmission: Transmission can likely occur from direct contact with infected snakes or from an environment contaminated with O. ophidiicola. Skin abrasions may facilitate O. ophidiicola’s ability to cause infection.
Clinical signs: Experimental infections have shown a progression from swelling at the site of infection to raised scales, areas of scale discoloration, and erosion/ulceration of the skin. Behavioral changes associated with SFD include more frequent shedding of skin (ecydsis) and increased basking time; both are likely mechanisms employed to fight infection.
Diagnosis: While gross lesions of skin swelling, discoloration, or erosion can be suggestive of SFD, other causes of skin disease in snakes can result in similar gross lesions. Characteristic microscopic lesions include epidermal necrosis, often affecting only the superficial to mid-epidermis, which contain 2- to 5-um diameter parallel-walled, septate, branching, fungal hyphae. Characteristic 2- to 5-um rectangular arthroconidia can occasionally be found on the skin surface. The dermis may be unaffected or may contain mononuclear to granulocytic inflammatory cells, or fungal granulomas. Internal lesions, such as the fungal granulomas in the lung in this case, are less common. Fungal culture or PCR can be used to identify the organism. Because Oo has been detected on the skin of snakes without lesions of SFD, histopathologic evidence of infection is required for a diagnosis. A case definition of SFD has been proposed.
Wildlife population impacts: Snake fungal disease has the potential to negatively impact vulnerable snake populations that are threatened by other causes, such as eastern massasauga rattlesnakes, timber rattlesnakes (Crotalus horridus), and Lake Erie watersnakes (Nerodia sipedon insularum).
References
- Amanda CD, Matthew CA, Vincent H, Carol WM. 2014. Systemic Ophidiomyces ophiodiicola infection in a free-ranging plains garter snake. Journal of Herpetological Medicine and Surgery. 24(1):7-10. https://doi.org/10.5818/1529-9651-24.1.7
- Baker SJ, Haynes E, Gramhofer M, Stanford K, Bailey S, Christman M, Conley K, Frasca S, Ossiboff RJ, Lobato D, Allender MC. 2019. Case definition and diagnostic testing for snake fungal disease. Herpetological Review. 50(2):279-285.
- Franklinos LHV, Lorch JM, Bohuski E, Rodriguez-Ramos Fernandez J, Wright ON, Fitzpatrick L, Petrovan S, Durrant C, Linton C, Baláž V, Cunningham AA, Lawson B. 2017. Emerging fungal pathogen Ophidiomyces ophiodiicola in wild European snakes. Sci Rep 7, 3844. https://doi.org/10.1038/s41598-017-03352-1
- Ladner JT, Palmer JM, Ettinger CL, Stajich, JE, Farrell TM, Glorioso BM, Lawson B, Price SJ, Stengle AG, Grear DA, Lorch, JM. 2022. The population genetics of the causative agent of snake fungal disease indicate recent introductions to the USA. PLOS Biology 20(6):e3001676. https://doi.org/10.1371/journal.pbio.3001676
- Lorch JM, Knowles S, Lankton, JS, Mitchell K, Edwards JL, Kaofer JM, Staffen RA, Wild ER, Schmidt KZ, Ballmann AE, Blodgett D, Farrell TM, Glorioso BM, Last LA, Price SJ, Schuler KL, Smith CE, Wellehan JFX, Blehert DS. 2016. Snake fungal disease: an emerging threat to wild snakes. Philosophical Transactions of the Royal Society B: Biological Sciences. 371(1709):20150457. https://doi.org/10.1098/rstb.2015.0457
- Lorch JM, Lankton J, Werner K, Falendysz EA, McCurley K, Blehart DS. 2015. Experimental infection of snakes with Ophidiomyces ophiodiicola causes pathological changes that typify snake fungal disease. ASM Journals. mBio. 6(6):10.1128/mbio. 01534-15. https://doi.org/10.1128/mbio.01534-15
- Thompson, NE, Lankau, EM, Rogall, GM. 2018. Snake Fungal Disease in North America: U.S. Geological Suvey Updates. U.S Geological Survey Fact Sheet 2017-3064. https://doi.org/10.3133/fs20173064.
- USGS National Wildlife Health Center. 2019. Snake fungal disease in a Black Racer snake. https://www.usgs.gov/news/pathology-case-month-black-racer-snake Accessed July 2023.